

Reticulocytes appear greenish-blue and have different concentrations of reticulum formation.Keep the record of reticulocytes as well.Try to make a thin smear with around 100 cells per field.Count a total of 1000 RBCs under the 100 x oil immersion lens.Now make three thin smears and let them dry.Resuspends the cells before making the slides.Incubate the mixture for 10 minutes at 37 ☌.If Hb is low, then add one more drop of blood.Add two drops of blood to three drops of NMB solution.The procedure of NMB stain (reticulocytes stain): Mix these three reagents for at least 15 minutes, filter, and store them at room temperature.The staining visualizes reticulocytes with vital dyes like methylene blue that precipitate the RNA and organelles, forming a reticulum network.This new methylene blue stain is more specific for the reticulocytes.New Methylene blue stain (NMB) for reticulocytes count. In contrast to red-orange RBCs, reticulocytes in Wright’s stains look gray or blue-gray this condition is called polychromatophilia.When present in sufficient numbers, it may give rise to an increase in MCV. Reticulocytes are larger than normal RBCs and may be recognized as macrocytes.Reticulocytes need special vital stains like new methylene blue or cresyl blue stains.These are recognized as immature red blood cells in the peripheral blood smear.Reticulocytes are not easily visible with the Wright or Giemsa stain.Maturation abnormalities like microcytic or macrocytic anemia.>3% reticulocytes indicate hemolytic anemia, indicating compensatory bone marrow response.
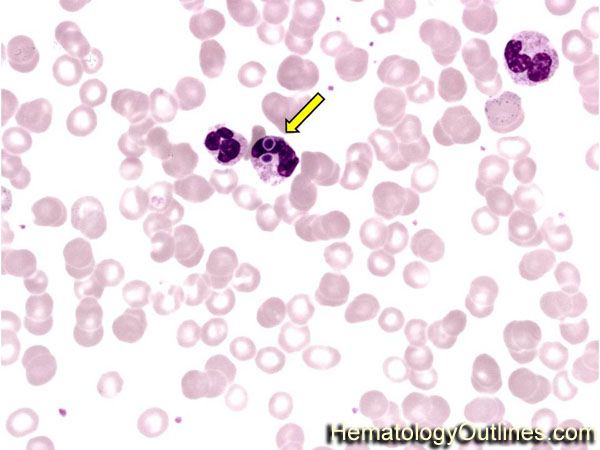
Anemia typing and diagnosis can be made on reticulocytes count.Elevated reticulocytes in the presence of normal hemoglobin indicate erythrocyte activity.Reticulocyte count importance (functions): In the case of anemia, hemoglobin will fall, and the circulating RBCs number will fall, while the reticulocytes number will increase.This will be due to defective or decreased bone marrow production or a decreased amount of erythropoietin. When hemoglobin is low and reticulocytes are 0.5 to 2.5%, it will indicate that anemia’s response is inadequate.RBC mature form circulates in the peripheral blood for 120 days.This indicates normal bone marrow activity when hemoglobin is normal. 0.5 to 2.5% are the normal reticulocytes in the peripheral blood.Reticulocytes circulate in the peripheral blood is 1 to 2 days.Bone marrow replaces approximately 1% of the adult RBC every day.Reticulocytes’ average life span = 1.0 days in the peripheral blood.RBC average life span = 100 to 120 days in the peripheral blood.When RBCs are released into the peripheral blood, they contain reticular material, which remains 1 to 2 days before the cell fully matures.Life of reticulocytes in the peripheral blood and bone marrow response: These large RBCs containing ribosomal RNA material look like reticulofilamentous material giving the name reticulocytes.This is the microsomal and ribosomal material left in the RBCs.The reticulocytes contain the reticular material, which is basically RNA, and it stains grey-blue (Aggregates of ribosomal RNA) with supravital stains like new methylene blue or brilliant cresyl blue.Reticulocytes are nonnucleated, fully hemoglobinized RBCs.The reticulocytes are young, immature, nonnucleated RBCs.Reticulocytes are present in between the nucleated RBCs and mature peripheral blood RBCs.Pregnancy may cause an increase in the reticulocyte count.Even the machine can count these as reticulocytes and give a false count. Howell-jolly bodies may be mistaken as reticulocytes.RBC inclusions may be mistaken as reticulocytes like Pappenheimer bodies, basophilic stippling, or Heinz bodies.Avoid counting insufficient numbers of RBCs and reticulocytes.Check bone marrow function in chemotherapy, radiation, and bone marrow transplantation patients.To find out the effect of the radioactive material on exposed workers.To assess the recovery of bone marrow function in aplastic anemia.To check the effectiveness of Pernicious anemia, folate, and iron deficiency treatment.Reticulocyte count differentiates anemia caused by bone marrow failure, hemorrhage, or hemolysis.Collect 5 to 7 mL of venous blood in the lavender-top tube.


 0 kommentar(er)
0 kommentar(er)
